Government Mandates Jacking Up Health Care Costs
Have you noticed that the mail from your health insurance company weighs a little more these days? Ever wonder why there are several pages of disclaimers in just about everything we send? Turns out, all that extra paper is the result of a government mandate that requires health plans – like CDPHP® – to tell our members that we don’t discriminate. The requirement, one last curtain call of the Affordable Care Act (ACA), also calls for plans to provide this information in at least 15 non-English languages that are most prevalent in the states where we operate.
Pages and pages of disclaimers merely scratch the surface. Let’s take a look at all of the ways government regulations impact the price you pay for health care.
Save a Tree? Not So Fast!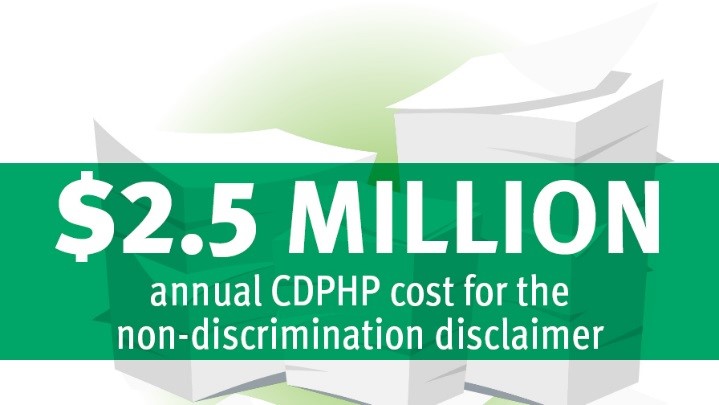
On the surface, it sounds like a good idea for health insurers to reassure their members that they don’t discriminate and provide them with information in a language they can understand. The problem, however, is that the regulation – section 1557 of the ACA – is wasting reams of paper and adding millions of dollars to the cost you pay for health insurance.
The disclaimers, which amount to two extra sheets of paper, must be included in “all significant communications” that we send to our members. That means every letter, notice, newsletter, contract, bill, or brochure contains a disclaimer. And no, we are not allowed to simply post this information on our website.
Early estimates forecast that this regulation alone will cost CDPHP $2.5 million dollars more per year.
Extra Paper is Just the Beginning
The extra paper isn’t the only factor that’s jacking up the cost of health care. Each year, state and federal lawmakers pass dozens of laws and mandates, most of which are well-intentioned, but often lead to higher costs.
Twenty years ago, New York passed the Health Care Reform Act (HCRA), with the goal of ending state-imposed price controls on hospitals. The law’s intentions were good but they le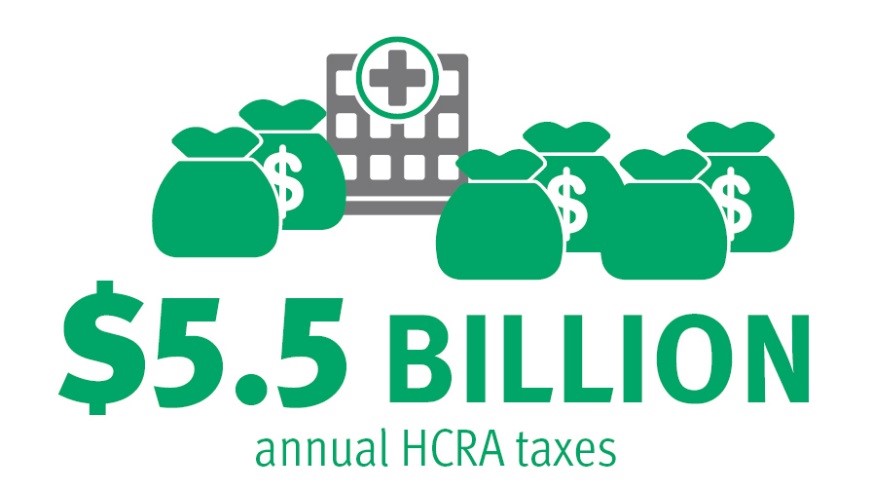 vied a hefty tax on health insurers to – in part – pay for the charity care that hospitals provide. Over the past two decades, HCRA taxes have ballooned to a whopping $5.5 billion a year and now rank as the third-largest tax in the nation’s highest-taxed state. Try to say that five times fast!
vied a hefty tax on health insurers to – in part – pay for the charity care that hospitals provide. Over the past two decades, HCRA taxes have ballooned to a whopping $5.5 billion a year and now rank as the third-largest tax in the nation’s highest-taxed state. Try to say that five times fast!
To make matters worse, funds collected from the HRCA tax haven’t even been used effectively. The Empire Center for Public Policy recently released Hooked on HCRA: New York’s 20-Year Health Tax Habit, a report that states, “HCRA funds pay for questionable purposes that do not directly contribute to improving patient care or broadening coverage.” The report goes on to say, “In the name of ‘reform,’ New Yorkers struggling to afford health coverage are paying billions in regressive taxes to finance programs that do little to improve health care – and, in some cases, enable dysfunction.”
Many of the law’s provisions are set to expire at the end of 2017. The Empire Center is pleading with state lawmakers to use this as an opportunity to trim the fat from the law and redirect funding to programs that improve the quality of care here in New York.
When Drugs and Politics Collide
Then there’s the recently passed step-therapy law. The mandate requires health insurers to provide an expedited review of prescription drugs that are subject to step-therapy requirements. Step  therapy is a drug management tool that health plans use to protect consumers from drugs that are new to the market, have not been proven safe for long periods of time, and are not the most cost-effective option.
therapy is a drug management tool that health plans use to protect consumers from drugs that are new to the market, have not been proven safe for long periods of time, and are not the most cost-effective option.
With drug costs rising an average of 13 percent per year, health plans use step therapy to control costs. The law allows doctors to undermine these efforts and will ultimately lead to consumers paying higher copays, deductibles, and eventually premiums. According to the New York Health Plan Association, the law could increase the cost of prescription drugs in the state by as much as $530 million.
It is important to understand that less than 1 percent of medications have a step-therapy requirement and that our plan works closely with local, practicing physicians to make decisions about prescription drug coverage.
The Big Picture
The fact of the matter is that government – while often well-intentioned – has a way of creating policies that lead to higher costs. In fact, 7 percent of every dollar you spend on health insurance goes directly to government taxes and fees. 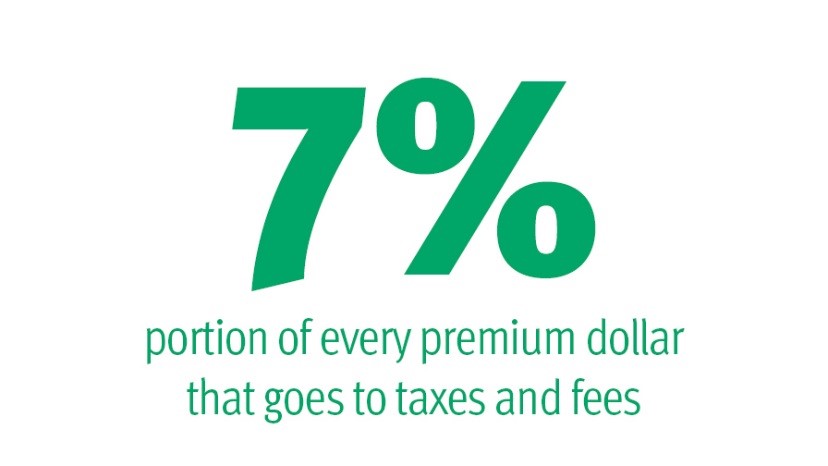
President Trump recently signed an executive order calling for a rollback of federal mandates, saying he would “knock out two regulations for every new regulation” enacted. While it remains to be seen which regulations the president plans to eliminate, I’m optimistic that elected officials have begun to see that future policies must be designed with affordability in mind.
 The Daily Dose
The Daily Dose
Carolyn Malone
I appreciate the fact that CDPHP is mandated by law to send discrimination notices and appeal notices with EOB’s but with weekly allergy shots I can fill a trash can with all the excess paper. Why can’t multiple EOB’s be sent say on a monthly basis with one set of the required additional papers. Also why not offer the option of patients receiving EOB’s by email. Then the patient can opt to save to a file or print them. Think of the trees saved as well as the costs.
John D. Bennett, MD, FACC, FACP
Hi Carolyn,
Thank you for your comment.
Unfortunately, government regulation prevents us from combing EOBs or non-discrimination notices. We are, however, working toward a paperless solution. The process is quite complex given regulations, but we hope to have a solution in the near future. In the meantime, I would encourage you to log into your account on CDPHP.com, where you can access claims files and much more.
Thank you,
Dr. John Bennett