Antibiotics Aren’t Always the Answer
Nobody wants to be sick. And when we are sick, we want the doctor to fix us. But insisting on an antibiotic for a common cold, the flu—or even bronchitis—is not always the answer. 
Antibiotics are powerful medications, but they are losing effectiveness because they are often used inappropriately. As the Centers for Disease Control and Prevention (CDC) reminded us during U.S. Antibiotic Awareness Week, most cases of bronchitis are caused by viruses, not bacteria. And antibiotics do not help treat viruses. The key is to talk to your doctor about the right course of treatment for your illness.
In addition, these medications are not without side effects, some of which can be pretty nasty. Taking antibiotics when they are not needed can lead to diarrhea, rashes, and stomach pain. More severe (but rare) side effects can include serious allergic reactions and kidney issues.
Worst of all, using an antibiotic when you don’t need one will encourage the development of antibiotic-resistant bacteria that can spread among family members, schoolmates, and co-workers—threatening your community with a new strain of microbes that are more difficult to cure and more expensive to treat. The consequences can include longer-lasting illnesses, more doctor visits, intravenous antibiotics, and hospitalizations. Some resistant infections can even be deadly.
Keep these antibiotic safety pointers in mind: 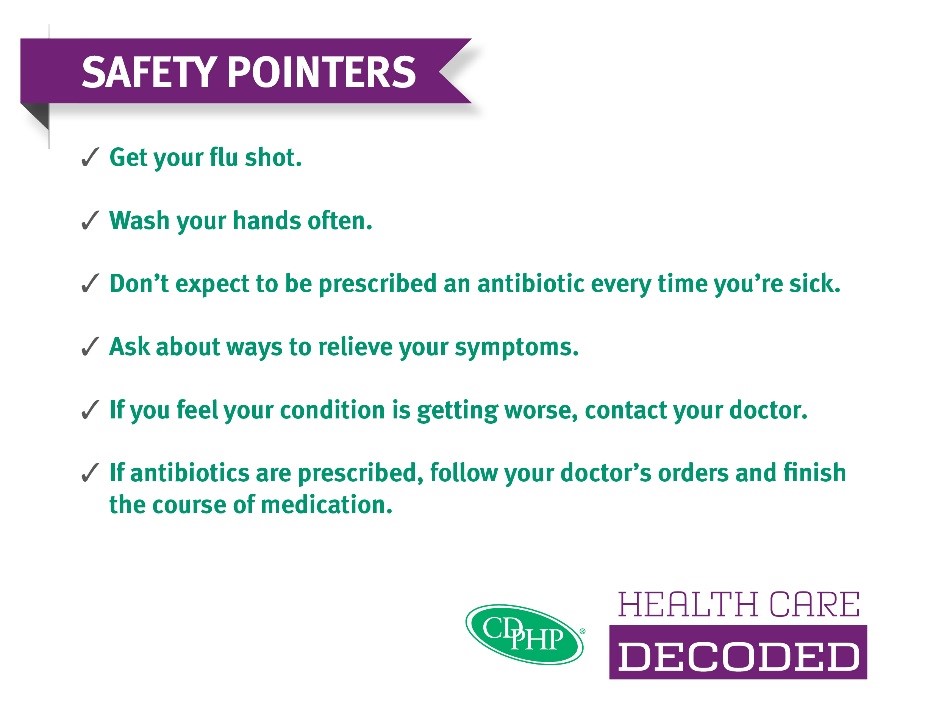
- Get your flu shot. This will go a long way in keeping you healthy year-round. For many CDPHP members, flu shots are covered in full. We also recently debunked several myths surrounding flu shots. Join the CDPHP Flu Shot Squad today!
- Prevent the spread of germs by washing your hands often. Antibacterial cleaners aren’t necessary. Plain soap and water work fine to kill most germs.
- Don’t expect to be prescribed an antibiotic every time you’re sick. Most cases of bronchitis, common colds, and the flu should not be treated with antibiotics unless your doctor determines that your condition is complicated by a bacterial infection.
- Ask about ways to relieve your symptoms, such as rest, fluids, and over-the-counter remedies.
- If you feel your condition is getting worse, contact your doctor.
- Finally, if antibiotics are prescribed, follow your doctor’s orders and finish the course of medication. Never try to save antibiotic pills or share them with friends.
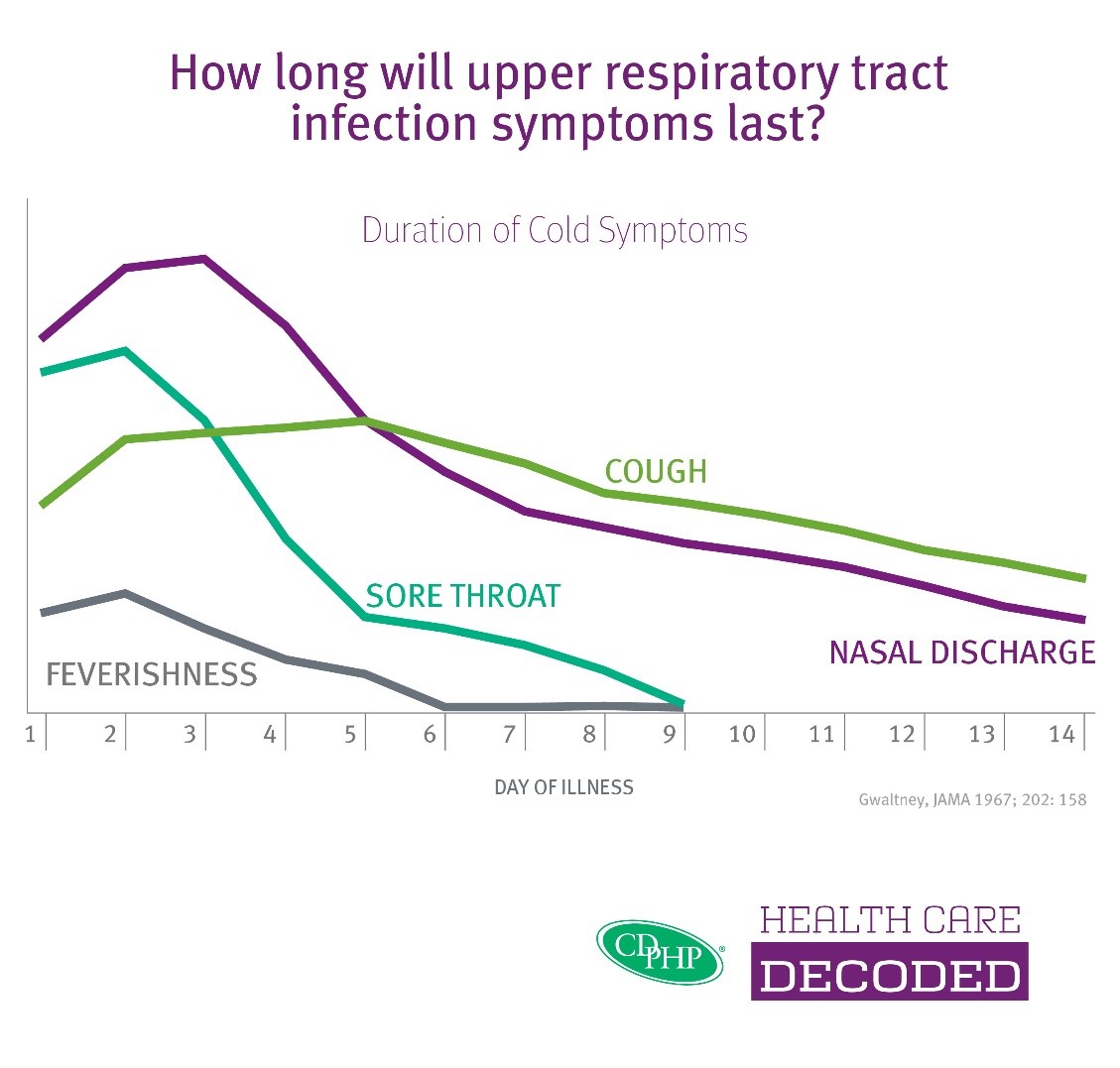
Remember, your cough or nasal discharge may last two weeks or more. Refer to the chart below whenever you are sick to assess your symptoms.
 The Daily Dose
The Daily Dose
Comments are closed.