Cervical Cancer Screenings Save Lives

A simple phone call might have saved Shari’s life. A CDPHP community health specialist called Shari and offered to help her set up an appointment for a cervical cancer screening, commonly known as a Pap test. Shari decided that there was no time like the present and picked a day and time to see her OB/GYN.
The results of her Pap test were abnormal, so Shari made several follow-up appointments, one of which determined that the abnormality was a precancerous growth. Fortunately, the growth was successfully removed in time, and Shari is alive and well. She concluded that she owes her good health to that phone call.
“It saved my life,” she recently told the community health specialist.
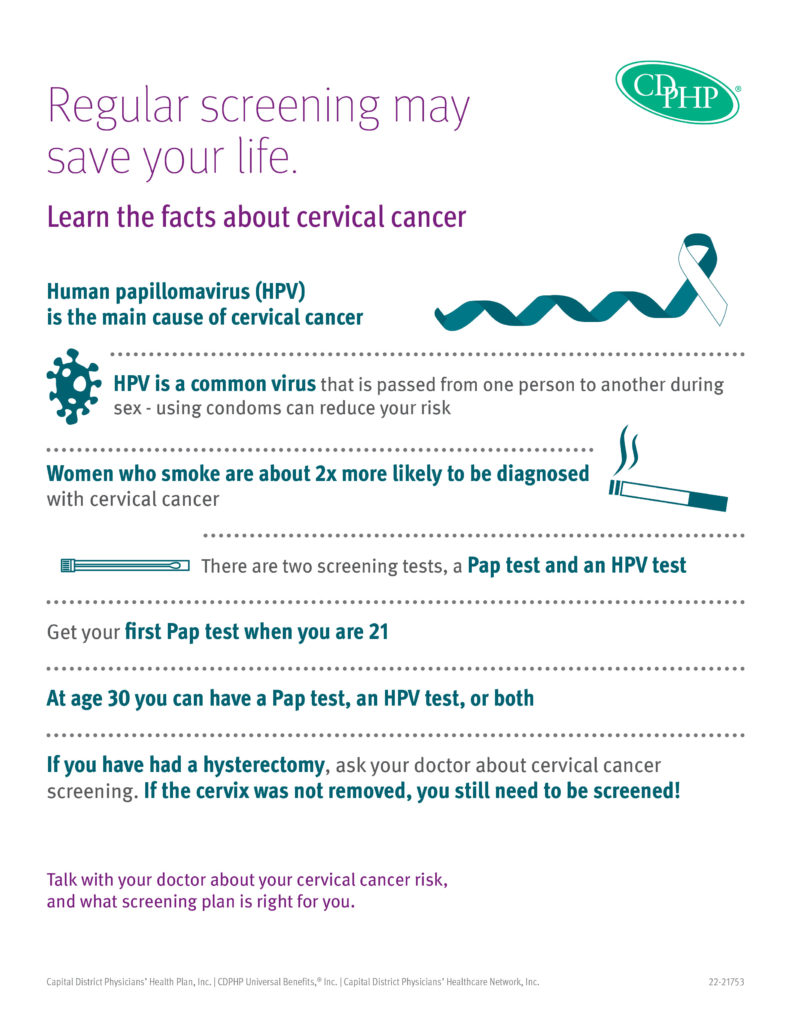
Cervical Cancer Risk Factors
Certain risk factors can increase a woman’s chances of developing cervical cancer, including:
- Human papilloma virus (HPV) infection: HPV can be spread through skin-to-skin contact, including sex. HPV infections are common and most people’s bodies can recover without treatment; however, if the infection becomes chronic, it may eventually cause certain cancers, including cervical cancer. Although doctors believe that a woman must have had HPV for cervical cancer to develop, most women with the virus do not develop it.
- Smoking: Women who smoke are about twice as likely to get cervical cancer as non-smokers. Tobacco by-products are absorbed through the lungs and carried in the bloodstream throughout the body, sometimes ending up in the cervical mucus. Doctors believe that these substances damage the DNA of cervix cells and may lead to the development of cervical cancer. If you smoke, keep in mind that it’s never too late to quit. CDPHP offers quitting smoking resources that can help you overcome your addiction.
- Weakened immune system: The immune system is vital for destroying cancer cells and slowing their growth and spread. HIV, drugs used to treat autoimmune disease, and organ transplants may weaken, and in the case of HIV, damage the immune system and increases a woman’s risk for HPV infections, as well as cervical cancer.
- Chlamydia infection: Women who are currently infected with chlamydia or have had a past infection may have a higher risk of developing cervical cancer. As symptoms are often not present, most women may not know that they are infected unless they are tested via a simple urine screening. While there is no vaccine for chlamydia, treatment generally entails a round of antibiotics.
- Family history of cervical cancer: If a woman’s mother or sister had cervical cancer, her chances of developing it are two to three times higher. Some doctors believe that this tendency is caused by an inherited condition that reduces a woman’s ability to fight off an HPV infection. In other instances, women with a family history could be more likely to have one or more of the non-genetic risk factors described above.
Cervical Cancer Screenings Save Lives
According to the American Cancer Society, cervical cancer can be found early, and sometimes prevented entirely, through regular Pap and HPV tests. These screenings can also detect pre-cancers so that they are treated before they become cervical cancer. Most invasive cervical cancers are found in women who have never had a Pap test or who have not had one recently.
When detected early, cervical cancer is one of the most successfully treatable cancers. In fact, thanks to the effectiveness of the Pap test, the cervical cancer death rate in the U.S. actually declined by more than 50 percent over the last 30 years.
CDPHP Covers Cervical Cancer Screenings
As part of its comprehensive benefit plans, CDPHP covers these life-saving screenings in full when provided by an in-network doctor, and members do not need a referral from their primary care physician. To find a participating doctor who offers Pap tests, use our Find-A-Doc search tool.
Our screening guidelines are as follows:
| Recommendation | Age |
| First Pap test; Pap tests aren’t needed for women 16 – 20 unless there are special circumstances. | 21 |
| Pap test every three years, as long as the test results are normal. | 21 to 64 |
| Pap test every five years when paired with an HPV co-test. | 30 to 64 |
| No additional Pap tests needed, but pelvic exams are still recommended; doctors should make that determination. The exception is for a woman who had a serious precancerous change to her cervix at some point in her life. | Older than 65 |
| Pap tests are no longer needed after a total hysterectomy that includes removing the cervix; however, vaginal pap smears may still be done after a total abdominal hysterectomy when cancer was the reason. | All ages |
Don’t put it off; schedule your screening today.
 The Daily Dose
The Daily Dose
Comments are closed.