Understanding Electronic Health Records
What are Electronic Medical Records and Electronic Health Records?
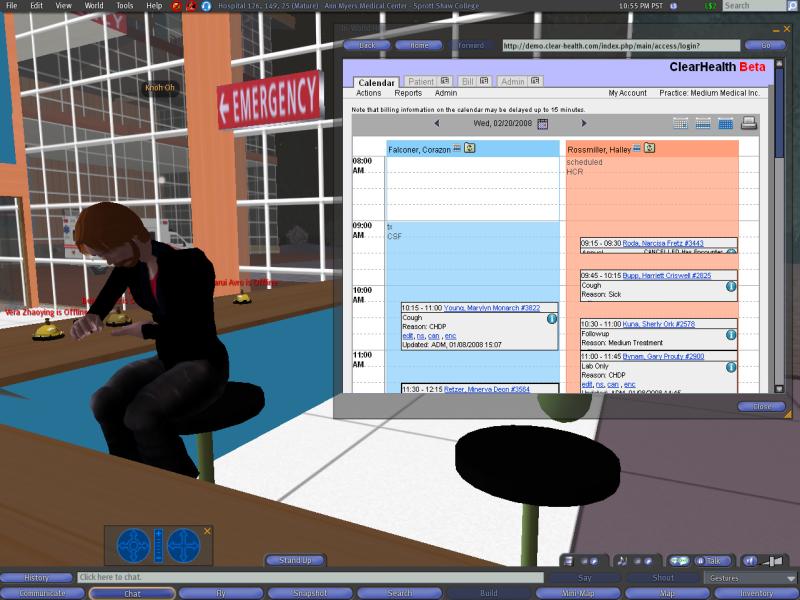
Every time you visit the doctor or a hospital, notes are made in your patient chart — everything from the way you present to the doctor or nurse to what your diagnosis is and what prescriptions were written. We have all been asked to complete a patient medical history form before a procedure, or even at routine office visits. If you visit more than one physician regularly, or if you have had various doctors throughout your lifetime, your medical records likely exist in multiple charts in different doctors’ offices. An electronic health record (EHR) is designed to streamline this process. In essence, it’s a systematic collection of patient health information in digital format that is able to be shared across various health care settings.
This way, the patient’s medical data is captured each time she or he visits the doctor, and the EHR allows for patient history to be consistently maintained, up-to-date and stored in a universal format.
CDPHP has promoted the use of this technology among our network providers for years. We also support the efforts of Hixny, a local not-for-profit that is helping medical practices connect with each other. If you are asked to sign a Hixny consent form at your doctor’s office, please rest assured that granting this access can only serve to enhance your care.
There is an important distinction between an EHR and an electronic medical record (EMR): An EMR is the record that is created and maintained in a single provider’s office. The EHR is a comprehensive patient history; it can be based on a doctor’s EMRs, but it is the EHR that travels with the patient to all providers involved in that patient’s care and that is used by multiple health care organizations.
What are the benefits to electronic health records?
Data tracking over time:
This can allow a physician to better understand a patient’s history and perhaps foresee future issues.
- Patient alerts: Depending on how a physician’s office uses EMRs, they could be used to alert patients when they need preventive visits or screenings.
- Convenience: An EHR can be a convenient way for a physician to quickly review and share a specific aspect to a patient’s medical history. For example, the physician could get a snapshot of the patient’s historic blood pressure readings in order to see if there are any patterns that might help in future treatment.
- Coordination of care: If a patient arrives at an emergency department in a life-threatening crisis, precious minutes can be saved if hospital staff are able to immediately access the patient’s complete medical history electronically, rather than attempting to treat the patient with no idea as to what prior or current conditions, allergies, or medications might be relevant. As well, the EHR can let hospital staff know who are the patient’s primary and specialty care providers so that those people can be efficiently consulted.
- Reducing test duplication: If a hospital or provider has access to a patient’s complete medical history, it could save time by referring to the record for data instead of awaiting test results before providing treatment.
- Efficiency: Physicians and other providers are busy people, as are patients. We all want to be in and out of the doctor’s office as fast as possible, but we still want our doctor to spend as much time with us as she or he can. EHRs can streamline a physician practice’s health care transactions — a physician with an EHR can usually transmit a prescription to the pharmacy before leaving the examining room so that it’s available to the patient immediately after the office visit, and office staff can sometimes submit insurance claims immediately while the patient is in the office. While these seem like small things, each extra efficiency that an office can have equals more time providers can devote to patient care.
- Legibility: If you’ve ever peeked over the doctor’s shoulder while he or she had your chart in hand, you know that handwriting can be close to impossible to decipher — even for other doctors. An electronic record can help reduce the likelihood of mistakes made because a chart has been misread or misinterpreted.
- Safety: Although any care provider — whether it’s a hospital, doctor, or pharmacy — should have built-in safeguards against medication dosage errors and harmful interactions, mistakes do occasionally happen. However, some EHR systems can be configured to flag a potentially dangerous drug interaction, verify medications and dosages, and check the patient’s allergy history, all of which can help improve patient safety.
- Accessibility: Especially if you have multiple physicians, having EHRs can help you take a more active role in your own health care. It should be easy for your provider to provide you a copy of your test results, medications, or X-rays or other diagnostic assessments. That way, you can bring a copy of an X-ray with you to a physical therapist, perhaps, or you can more closely monitor your own glucose levels. If you’re trying to coordinate your care between an allergist and endocrinologist, for example, an EHR can help each provider more fully understand how the others are treating your conditions.
- Security: You’ve undoubtedly been asked once or twice to sign a form acknowledging receipt of your provider’s Health Insurance Portability and Accountability Act of 1996 (HIPAA) policy. Part of HIPAA includes the Security Rule, which sets forth standards for how EHRs can be stored and transferred. That means that there are specific safeguards that are required by law for a provider to use in order to protect your information. HIPAA includes regulations with respect to what specific individuals are allowed to access personal information. For example, if you have a neighbor, family member, or acquaintance who works in the hospital where you receive treatment, and that person attempts to access your health information and is not authorized to do so, an “alarm” would be set off within the hospital’s computer system to alert administrators that the person inappropriately attempted to view patient records. As well, records are backed up securely and off-site. If a natural disaster happens, you need not worry that all of your medical records are gone — paper records in doctors’ offices can be destroyed in a flood or fire, but electronic records have many more levels of backup.
Electronic health records are most likely here to stay, though their formats and applications will likely change over time. You can ask your provider if she or he is using electronic medical records and, if so, how you can maximize your interaction with your records in order to best suit your health care needs.
References: HealthIT.gov, Centers for Medicare & Medicaid Services
 The Daily Dose
The Daily Dose
Comments are closed.