One of the Biggest Threats to Affordable Health Care
No one likes to go to the hospital, but when you do, you expect the best. The best care, the best technology, the best medicine, and certainly the best doctors.
Hospitals have become a mainstay of the American health care system, and frankly, a pillar on which most major cities are built. But despite the important role these medical institutions play in the communities they serve, the quality of care you receive at hospitals is being threatened by a quiet revolution.
In 2010, the Affordable Care Act (ACA) was passed with the goal of increasing access to affordable health care. While the law succeeded in its quest to get more people covered by health insurance, it also spawned a rash of hospital consolidations.
The law’s authors were convinced that consolidation would decrease costs by reducing duplicative services and better care coordination. In fact, Robert Kocher, Ezekiel J. Emanuel, and Nancy-Ann M. DeParle wrote in the Annals of Internal Medicine that the ACA would “unleash forces that favor integration across the continuum of care.” And so it did…
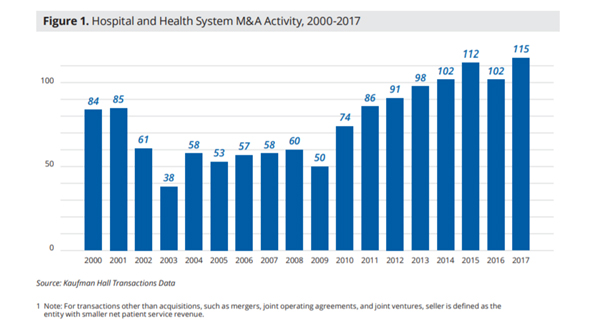
Two years after the ACA was signed into law, the Heritage Foundation reported a sharp spike in hospital consolidations, with 100 mergers and acquisitions in 2012 alone. Since then, consolidation has shown no sign of slowing, with 115 transactions in 2017, a 13 percent spike from the previous year. The below chart by Kaufman Hall shows the steady climb in hospital and health system mergers since the ACA was passed.
Most hospital execs will argue that consolidation improves efficiencies and lowers costs. But a recent study by the American Journal of Managed Care found that health care markets dominated by large hospital systems had both higher health care costs and higher insurance premiums. The data is not surprising when you consider the fact that consolidation gives hospitals greater negotiating power against health insurers, like CDPHP. As a health plan, our job is to negotiate with hospitals to ensure our members are getting the very best prices. But if hospitals are allowed to leverage their massive buying power to jack up rates, patients lose.
In addition to hurting consumers in the form of higher costs, consolidation also hurts the independent practice of medicine. Lured in by the promise of a larger system that can afford to comply with changing regulations and sky high technology updates, a number of independent doctors have also been sucked up by the storm. According to the Journal of American Medical Association, patients treated by physicians who are employed by hospitals pay 20 percent more than those treated by independent doctors.
As a physician-founded health plan, CDPHP is deeply committed to the independent practice of medicine. We know that doctors do their best when they’re empowered to make decisions at a local level. Locally and nationally, we understand that the urge to merge is stronger than ever, but we will continue fighting the negative effects of consolidation, and working to offer you, your family, and your business the highest-quality care at the most affordable price.
 The Daily Dose
The Daily Dose
Comments are closed.