The Power of Cost Transparency

Health insurance remains the single most important benefit to job seekers today. That’s according to a recent survey by Glassdoor, which found that medical and dental benefits are more important to applicants than vacation time, bonuses, and even retirement packages.
While the number of businesses offering health insurance remains steady, the cost of care is skyrocketing. Over the last decade, the cost of family coverage has jumped 70 percent, far outpacing the rate of inflation. In order to combat these trends, some employers have begun turning to insurance companies for ideas about how to improve employee health, and subsequently, lower costs.
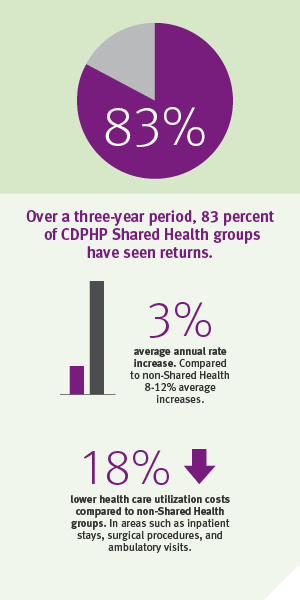
Enter: CDPHP Shared Health. Over a three-year period, 83 percent of Shared Health groups have seen returns. They have seen rate increases of 3 percent, compared to 8-12 percent increases non-Shared Health groups are experiencing. They also, on average, see 18 percent lower utilization costs, in areas such as inpatient stays and surgical procedures.
Available to large businesses, CDPHP Shared Health allows for the combination of enhanced workplace wellness initiatives and increased transparency to gain control of health care costs. With significant investments in analytic capabilities, CDPHP shares data with CDPHP Shared Health groups in the form of aggregated medical claims and personal health assessments, to identify cost drivers and savings opportunities. By meeting regularly with CDPHP clinical account executives and CDPHP health promotion specialists, groups can develop customized strategies, and review and improve programming. This level of transparency is unprecedented, and helps employers understand the factors that influence utilization, enabling informed decisions about workplace programming and benefits provided.
For example, if claims show that a large number of employees are not taking advantage of preventive screenings – such as getting a mammography, a colonoscopy, or attending an annual well visit – an employer can offer employees paid time off to complete these screenings. If claims show a high volume of employees using brand name prescription drugs, the company can educate its workforce about the savings associated with generic medications. And, if personal health assessment data shows a large number of employees using tobacco products, the company can offer its employees access to a tobacco-cessation program.
It is very important for employees to understand that this data, which is ONLY available in aggregate form, is not designed to single out any individual employee, but rather identify opportunities to improve the overall health of a workforce, thereby reducing the company’s health care spending.
Of course, not all companies participating in CDPHP Shared Health are instantly healthier, nor can all costs be controlled. The key is the combination of wellness and transparency that CDPHP Shared Health is able to offer clients, enabling them to focus on what they can change, mitigating the effects of what they can’t. Commitment is also significant, particularly participation for a minimum of three years, so that employer groups have a chance to really explore what works for them.
To get results, CDPHP Shared Health groups know that employees – at ALL levels – must participate. CDPHP Shared Health groups that have committed to the program’s philosophy have buy-in that starts all the way at the top.
To learn more, visit CDPHP. And, if you think CDPHP Shared Health is right for your large business, contact your broker or CDPHP representative today.
 The Daily Dose
The Daily Dose
Comments are closed.