Understanding Your Health Insurance ID Card
You may not think about your health insurance ID card very often. After all, it probably spends most of its time in your wallet—until you, your doctor, or another medical provider really need it.
Let’s take a minute, though, to look at the many important pieces of information you can find on your card. After all, it’s your passport to care and coverage, so you should know what all of the fields of information really mean.
The descriptions below apply to most private health insurance ID cards in the United States. If you live outside the U.S. or have government-provided insurance, you may see some different fields on your card. CDPHP® is dedicated to helping you understand your health insurance, but you should always call your own insurer at the customer service number on your card if you have questions about your specific health plan or coverage.
Most health insurance cards contain straightforward identification information about the people covered and the policy you have.
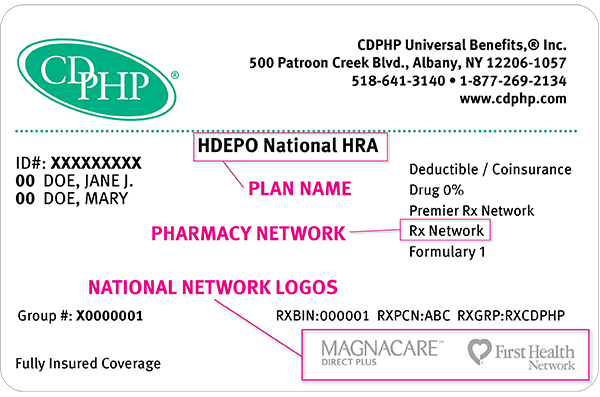
Carrier and Contact Information
This is the name of your insurance company and one or more ways to reach them, like their website and phone numbers for customer service or other specific needs. Some of this information may be on the back of the card.
Names of Covered Individuals
If you are the policyholder, your name will be on the card. If you have dependents—like a spouse or children—on your health insurance policy, their names might be listed on your card, too. If you are not the policyholder, then your card may show your name and the policyholder’s name in separate fields.
Member ID/Policy Number
Each person covered by a health insurance plan has a unique ID number that allows healthcare providers and their staff to verify coverage and arrange payment for services. It’s also the number health insurers use to look up specific members and answer questions about claims and benefits. This number is always on the front of the card. If you’re the policyholder, the last two digits in your number might be 00, while others on the policy might have numbers ending in 01, 02, etc.
Group Number
Each employer that purchases a health plan for its employees also has a number. This group number identifies the specific benefits associated you your employer’s plan. Healthcare providers use the group number plus your member ID number to file claims for your care. If you purchase insurance through a healthcare exchange (the marketplaces set up by the Affordable Care Act, sometimes called “Obamacare”), you might not have a group number.
Plan Type/Plan Name
There are many different kinds of health insurance plans. Insurance companies list the type of plan on your ID card to help healthcare providers file claims properly. For some plan types, the plan type will be listed on the ID card (example: HMO), while Medicaid and Child Health Plus cards will feature each program’s respective logo. Each plan type has different ways of handling referrals, in- and out-of-network providers, and out-of-pocket costs. The most common types are:
- HMO (health maintenance organizations)
- PPO (preferred provider organizations)
- EPO insurance plans (exclusive provider organizations)
- HDHP (high deductible health plans)
- Essential Plan
Some insurance companies give specific names to certain plans, like those available through the healthcare exchange, instead of using group numbers (above).
Payment Information
Many health insurance cards show the amount you will pay (your out-of-pocket costs) for common visits to your primary care physician (PCP), specialists, urgent care, and the emergency department. This may be a flat rate (copay) or a percentage of the cost (coinsurance). If you see two numbers, the first is your cost when you see an in-network provider, and the second—usually higher—is your cost when you see an out-of-network (OON) provider. For example, when you’re referred to a specific specialist or sent to a specific hospital, they may not be in your insurer’s network.
Medical Network
Your insurance company may provide out-of-area coverage through a different health care provider network. If so, the name of that network will likely be on your insurance card. This is the network you’ll want to seek out if you need access to healthcare while you’re away on vacation, or out of town on a business trip.
Prescription Benefits
If your plan includes benefits for prescription drugs, you will also find some information related to them on your health insurance ID card.
Formulary
The formulary is the list of prescription drugs that your insurance company covers. Some insurers have different formularies that are covered under different plans—and they indicate which formulary on members’ ID cards. For example, CDPHP members will see Formulary 1, Formulary 2 or the Medicaid Formulary on their cards. (If you are a CDPHP member with no formulary listed on your card, you have Formulary 1.)
Prescription Costs
Most formularies are divided into three tiers containing different types of drugs. Each tier is set at a different price that you’ll pay when you pick up your prescription at a participating pharmacy. Usually, generic drugs make up most of Tier 1, brand name drugs cost a bit more and make up most of Tier 2, and specialty drugs (which cost the most) make up most of Tier 3.
Pharmacy Network
Different insurance plans sometimes cover different pharmacy networks. If so, this is likely to be on your insurance card. For example, CDPHP employer plans use a Premier network; CDPHP individual plans (like those through the healthcare exchange) use a Value network; and CDPHP plans for seniors use the Medicare network.
Rx BIN (banking identification number)
Your pharmacist will use this number to process your prescription. It indicates which company will reimburse the pharmacy for the cost of the prescription. Not all insurance ID cards contain this number, though.
Helpful Resources
That seems like a lot of information to pack onto a little rectangle—and it is! Still, you may find additional information on your card, such as:
- Important telephone numbers and addresses that allow your healthcare providers to call for information (such as coverage verification, claims questions, pre-authorizations, etc.)
- Hotlines to help you get specific help quickly (to report fraud, for example)
- Resources to help you find specialty care (chemical dependency services, etc.)
Remember: If you’re a CDPHP member, you can view your ID card online through our secure member site or using the My CDPHP Mobile app.
You can always call the customer service number on your card to ask any questions about the details of your plan.
 The Daily Dose
The Daily Dose
Margaret Ross
I enjoyed the article explaining what is on my CDPHP card. I would like to offer the following improvement to the card. The most important item, my member number, should appear in much larger type. It would help those of us who are aging and require reading glasses otherwise. Thank you.
Jennifer Brett-Hargis
Hello, Margaret. Thank you for your very insightful and useful comment. I will definitely pass that information along to the membership and billing department; it’s always great for us to hear such important feedback from our members!
Patti
what does OON mean on my ins card?
Jennifer Brett-Hargis
Hi Patti,
OON means out of network. It refers to all medical providers that aren’t in the CDPHP coverage area.
Morgan
What does “Plan Code” mean on my insurance card? Is it the same as a benefit code?
Jennifer Brett-Hargis
Thank you for your comment, Morgan. Because health insurance companies include different information on their ID cards, I suggest that you contact your health insurer’s member services department to find out what a plan code is. Let us know what you learn!
Maria
What it means on a insurance card ” one tier , two tier ?”
Jennifer Brett-Hargis
Thank you for your comment. Because the information on ID cards varies according to which health insurer you have, I suggest that you contact your insurance company. They should be able to help you. Good luck!
chloe
where is the group number located on my ontario health card
Jennifer Brett-Hargis
Hi Chloe,
Ontario is outside of our health insurance company scope. I advise contacting your health insurance company directly for help with this. Good Luck!
Duaa
Where can i find the group number
Jennifer Brett-Hargis
Thank you for your comment. While ID cards vary according to the health plan that designs them, the group number is a vital piece of information that should be included. For example, on CDPHP ID cards, the group number is located on the lower left side of the card and is clearly labeled. I hope this was helpful!
Piran Beloa Forcha
I have heard people say they have multiple family members on one insurance card. Are the other family members indicated the BIN number or person code ?
Jennifer Brett-Hargis
Thank you for your comment! While ID cards differ according to the health insurance company that administers them, if a person’s family members, or dependents, are covered under the same plan, each dependent is usually listed on the card under the main policy holder. For example, if John Smith’s wife and two children are covered under his health plan, their names will appear on the ID card as follows:
John Smith
Mary Smith
Sam Smith
Sally Smith
The BIN number is used by your pharmacy to process your prescriptions, and I believe the code you’re referring to is the member suffix. Each member of a family account will have the same ID number and a two-digit suffix to differentiate them. The subscriber is always 00 and typically the spouse is 01. The remaining dependents would follow suit.
I hope this helps!
Piran Beloa Forcha
Thanks so much, you explained everything with clarity.
Austin
All that my card says is Carrier, Policy, ID, and Issue. Is “Carrier”, the so called Group Number?
Jennifer Brett-Hargis
Thanks for your comment, Austin. Usually, the “carrier” field includes the name of your health insurance company. If you’re a CDPHP member and have additional questions, please call us at (518) 641-3700. Hope this helps!
camila
where can I find who the policy holder is and does it say it on my card?
Jennifer Brett-Hargis
Thanks for your comment, Camila. The policyholder is usually the first name listed on your member ID card. On CDPHP ID cards, policyholders are located right below the ID number on the left-hand side and include the “00” suffix. Hope this helps!
cj
where is my policy number?
Jennifer Brett-Hargis
Thanks for your comment, CJ. Typically, the policy number is your ID number, which is usually located at the top of your member ID card. Hope this helps!
Leslie Farley
Hi. Where do I find the group number or plan code number on my Gateway insurance card?
Jennifer Brett-Hargis
Thanks for your comment, Leslie. While your best bet is to call the Gateway member services number for the most accurate information, I can tell you that the group number should be clearly identified on your ID card (e.g., Group #: 12345678). On CDPHP ID cards, it’s located in the lower left-hand corner. Hope this helps!
stromsoe
great article. after going through, one can get a pretty straightforward idea about the health insurance cards. I think that it is a good idea to maintain an effective health insurance coverage. I think that the cards should also link the patient’s previous medical history.
thank you.
Rita Giandonato
I am looking for Insurance Cards that display Multiple Networks ID’s. For example a Cigna PPO card, with a claim address of Integra Health. This would not be a Cigna PPO plan, but a Commercial Other. How do you explain? Teaching staff how to register patients with Multiple Identification Cards.
Jennifer Brett-Hargis
Hi Rita,
Thank you for your comment. CDPHP insurance cards contain the logos of our network partners.
Mary
Hello! I went to the pharmacy today and they told me that I had the wrong card with me for my medication. The card I brought was plastic and much like the one you described. Was it expired or should I bring them the paper copy?
Jennifer Brett-Hargis
Hi, Mary! In order to make sure you have the correct ID card, please give our member services team a call at (518) 641-3700 or toll free at 1-800-777-2273.
Bernard R Smith
WhT does pref mean
Jennifer Brett-Hargis
Hi Bernard, thank you for taking the time to read our blog and contact us. I believe ‘pref’ is referring to the term ‘preferred’, which would mean an entity CDPHP has a relationship with and in most cases, gives members access to lower-cost or copay-free services.
roselyn
hi,where can i find the Subscriber/policy ID on my insurance card and where can i fine the planID
Jennifer Brett-Hargis
Hi Roselyn – thanks for reaching out! Your subscriber ID is the very first item listed on the left-hand side of your card – it says ID#:.
Your Group # is listed on the bottom left-hand side of the card – it should say Group#:.
If you have any other questions, try giving member services a call at the number listed on the front of your ID card.
shradha shrestha
what is reference number ?
Jennifer Brett-Hargis
Hi Shradha – Thank you for your question. We encourage you to reach out to your health plan’s member services department so that they may assist you with specific questions about your ID card and benefits.
sam
where can I find the employer and the employer number on my insurance card ??
Jennifer Brett-Hargis
It sounds to me like you’re talking about the Group Number? If so, that can be found on the bottom left corner on the front of your ID card. Please let me know if that is helpful.
Elmo
why does my bcbs card not have a group number
Jennifer Brett-Hargis
Hi, Elmo – thank you for reaching out! Please contact BCBS at the number listed on your ID card for more information on your specific plan.
Kim
Where is the policyholder on a United healthcare card
Jennifer Brett-Hargis
Hi Kim – Thanks for reaching out! We suggest you contact your plan at the number listed on your member ID card for information specific to your card and plan.
Adam Martin
hi,
How can i find the Subscriber/policy ID on my insurance card.
Jennifer Brett-Hargis
The subscriber or member ID can be found in the top left corner of the CDPHP ID card. It appears above the subscriber name(s), which are listed just below. Let me know if that was helpful.
janette Carr
Where do I find “issuer” on my insurance card? Thanks! Janette
Jennifer Brett-Hargis
Hi Janette – The issuer is generally your insurance company, so in this case, it would be CDPHP. Hope this helps!
Michelle Trotman
What does “BL#” mean on the Lincoln Financial Group Dental insurance card? Is that considered a policy number or that’s healthcare talk?
Jennifer Brett-Hargis
Hi Michelle – You’ll want to check with your dental carrier directly. Their contact number is usually located on your member ID card.
Mike
Are any of the numbers on the card or on the statement have any reference to the account number where the payment goes ?
Or in other words where do I find the account number to pay the bill ?
Why does it have to be made so difficult to pay the bill using the online banking ?
David Filkins
Hi, Mike – sorry to hear you’ve experienced frustration with online bill pay. Here is a resource that may help: https://www.cdphp.com/customer-support/pay-my-bill
Alex
Guys, If a person JUST knows the bin number, id membership, rx group, and pcn,
Can They Know which insurance company the card belongs to ?
David Filkins
Hi, Alex – I don’t believe it’s possible to identify an insurance carrier with just that information. You may want to reach out to your current or a past insurance carrier for help.
Sharon Demarco
Where would the member ID be on the card?
David Filkins
Hi, Sharon – It depends on your plan, but CDPHP, for example, lists member IDs in the upper left-hand corner of our member ID cards.
Tyler
Where do I find the plan ID
David Filkins
Hi, Tyler – The location of a plan ID will vary from carrier to carrier. For CDPHP plans, the plan name can be found in the middle of the card. I hope this helps!
Farheen
hi guys i have a united healthcare insurance and for my college they are asking me to provide policy holder information with name last name and number i have submitted twice but the said that when i am submitting my name it they are not accepting because its a personal insurance but its a government insurance so where can i find the policy holder information
David Filkins
Hi, Farheen – I would suggest contacting your carrier’s member services department for help with this situation. The number should be on the front or back of your member ID card.
Esther Alex
Where can I find the subscriber name on my card
David Filkins
Hi, Esther – The subscriber name is generally whoever holds the insurance policy, so it could be you or a spouse/domestic partner. Your best bet is to call member services to confirm with your insurance company.
Nikki
I’m filling out a new application for kancare and I have had insurance before through them it’s asking me what’s the case number can I find it on the card? If so we’re at?
David Filkins
Hi, Nikki – Thank you for reaching out. Insurance companies tend to use slightly different terms to identify their plans. Your best bet is to contact KanCare directly.