Coping with the Unexpected: Hemolytic Disease of the Newborn
“Is he your first?”
The nurses drawing my newborn son’s blood would often ask me this question, probably to distract me from the pain-filled cries that were tearing me up inside. No, Griffin is not my first child, but he is the first to have complex health issues at birth.
Though stressful thanks to selling our home, living in a tiny apartment, and building our forever home, my pregnancy was otherwise smooth sailing. Routine bloodwork at the 20-week mark did reveal that my body had created antibodies E and M, likely as a result of delivering my daughter via urgent cesarean section. I discussed this with my doctors and did some additional research on what their presence meant. Antibody E did have the potential to cause mild problems, but since this occurred in a small percentage of patients and there was nothing that could be done before delivery, I vowed not to spend my pregnancy worrying about it.
Griffin Joseph Burkart arrived on January 20, 2018. He was 8.1 pounds, 21 inches, and received an often unheard of Apgar score of 9/10. My husband, John, and I were elated. We already had a beautiful daughter, Mila, and now our son would complete our family.
Once on the postpartum floor, the parade of visitors to meet Griffin began. Everyone commented on how beautiful he was – beautiful, and calm. Griffin was so quiet and was peacefully snoozing the day away. The next day, newborn testing was done and that was when we got the news: Griffin’s bilirubin level was extremely high (this is commonly known as severe jaundice, or hyperbilirubinemia), likely causing his excessively sleepy state. The antibodies had launched an attack. Griffin’s pediatrician quickly ordered phototherapy, a treatment used to lower bilirubin levels in newborn babies. He would need to spend the night in an incubator in the nursery, and would be brought to me every two hours for feedings.

John and I were terrified and completely heartbroken, but the phototherapy did lower his levels enough to be with us the next day.
However, repeat testing showed that his bilirubin level crept back up to the danger zone, and once again, he spent the night in phototherapy, and once again, his level successfully came back down.
We were desperate to get back home to Mila and were released that day, but by the time our follow-up visit to our pediatrician came the next afternoon, his yellow color had intensified and he was lethargic. She immediately sent us to St. Peter’s for a blood draw to check his bilirubin level.
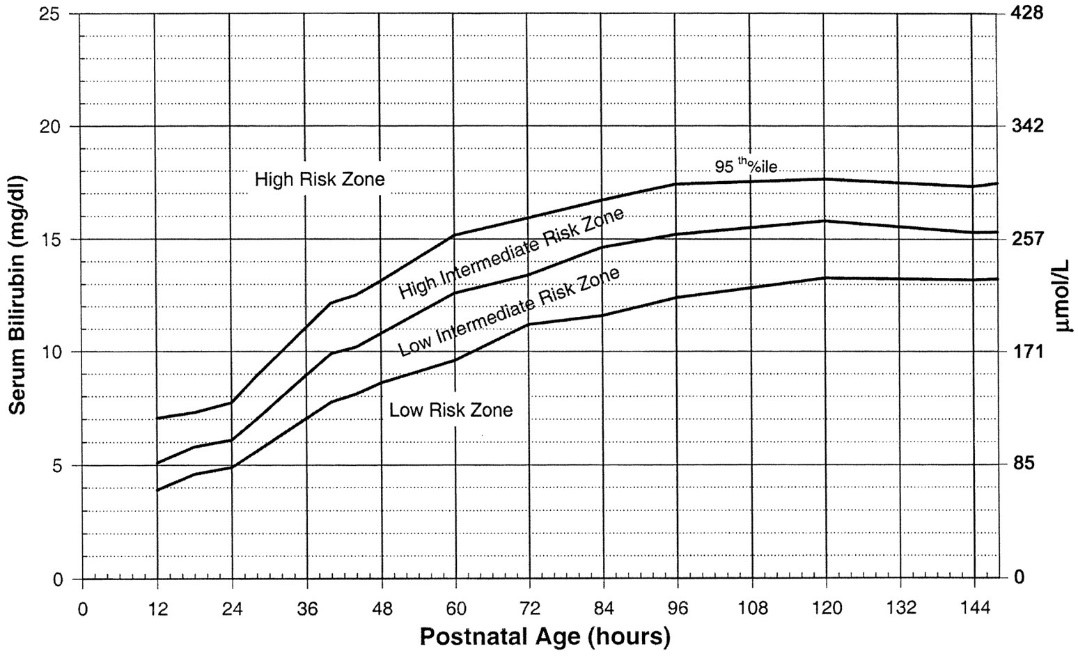
I received a flurry of frantic phone calls from our pediatrician and the lab – Griffin’s bilirubin level had shot up to a 21 (for reference, it should have been less than five). We were to return to St. Peter’s for a repeat blood draw immediately.
A repeat blood draw saw our worst fears realized: Griffin’s bilirubin level was now a 24. At 25 and higher, if left untreated, newborns run the risk of developing kernicterus, a serious condition that could cause hearing loss, neurological disorders such as cerebral palsy, and death.
Our pediatrician’s office went to work talking with the neonatologist at St. Peter’s to get Griffin started in intensive phototherapy as soon as possible. The nurses were already setting up an incubator with the phototherapy lights when we arrived upstairs. We made the decision to keep Griffin in the incubator full time to maximize the therapy’s effectiveness. We were told to be prepared to be in the hospital up to a week. I quickly asked the nursing staff for a breast pump so that I could maintain my supply and so that John and I could feed Griffin bottles while under the lights. I felt that if nothing else, I could at least continue providing my son with nourishment while we weathered this storm.

For the next four days, we watched our son lay in the incubator and held our breath for every blood draw, praying that his bilirubin level had gone down. Slowly but surely it did, and Griffin’s yellow color was replaced with beautiful, pink newborn skin. Finally, we got the news we’d been praying for: Griffin’s bilirubin level was a 10, completely normal for his age. We could finally go home. But just as I thought our nightmare was ending, a new problem was just beginning.
Toward the end of Griffin’s hospital stay, his hemoglobin, hematocrit, and reticulocyte counts were tested. We received a referral to follow up with the Melodies Center for Childhood Cancers and Blood Disorders at Albany Medical Center because the antibodies responsible for Griffin’s high bilirubin level were continuing to attack his red blood cells.
For the next two weeks, I would drive Griffin to Albany Medical Center three mornings a week for a blood draw and appointment with his pediatric hematologist. On Thursday, February 8, we found out that after just 24 hours, Griffin’s hemoglobin level had dropped more than a gram.
Adults can handle this type of fluctuation in their red blood cell count, but not two-week old babies. The antibodies attacking his red blood cells were doing so faster than he could create baby red blood cells of his own to replace them. Griffin would need to receive a blood transfusion as soon as possible. And he would possibly need two or three of them.
The blood transfusion took place on Friday, February 9. For about six hours, John and I passed our baby boy back and forth and held him while new, antibody-free blood entered his system. We returned to the hospital the following Monday to find that the transfusion had been successful: Griffin’s hemoglobin level had gone up. We were finally seeing a silver lining after so many dark clouds.
After several more weeks of trips to Albany Medical Center to monitor his hemoglobin level, on Friday, April 6, Griffin was discharged from the Melodies Center. His hemoglobin level had completely stabilized and the antibodies had finally lost their power over him. Our two-and-a-half month long nightmare had come to an end.

What I’ve Learned
It’s hard not to look back and wonder what I could have done to prevent this. The short answer, as his pediatric hematologist told me firmly, is nothing. There was no way to prevent the antibodies in my blood from attacking. But now that I’m a bit further removed from the experience, here’s what I would advise anyone who happens to find themselves in a similar situation:
Ask Questions
I cannot stress this enough. Ask all the questions. Do not rely on Google to help you understand what’s going on with you or a loved one. Everyone’s situation is unique. We are fortunate to have a hematologist in the family that we frequently referred to for second opinions. We trusted Griffin’s pediatric hematologist, but you can never have too much information when it comes to yours or a loved one’s health.
Understand Your Health Care Coverage
Even though I work for CDPHP®, I still failed at this. I know that certain services require members to call ahead for prior authorization, including inpatient hospital stays, but my brain wasn’t even capable of thinking of that at the time. Fortunately, I was able to file an appeal and have Griffin’s hospital stay for phototherapy approved after an initial denial. When I found out he needed a blood transfusion, I made sure to check my member contract before he had the procedure.
Use Your Support System
I’m not sure how I would have survived this time without John and our families. They took turns taking care of Mila, bringing us meals, and praying for Griffin’s recovery. If you find yourself dealing with complex health issues, please – ask for help. This isn’t the time to be a martyr. It’s a time to focus on healing and using your people to help you get there.
 The Daily Dose
The Daily Dose
Comments are closed.